The use of temporary hospital staff has become a key ethical issue for hospitals. It provides valuable flexibility, but its intensive use raises questions about efficiency, costs, and the impact on the quality of care. The challenge is not to “eliminate temporary staff,” but to make it complementary to a more sustainable organization.
How can replacement management be structured to ensure continuity of care, autonomy, and well-being for caregivers? And how can the urgent need for rapid replacement be reconciled with a sustainable HR policy? These questions call for a systemic response: better tracking, better anticipation, and expansion of the available pool of workers.
A more intelligent approach to replacement is being tested in order to strengthen the monitoring of staff and create structured alternatives to temporary work. Several levers are being mobilized: a dedicated portal, two-way feedback, a consolidated view of cumulative schedules, and institutional mobility.
Why temporary work becomes a risk when it becomes structural
When temporary work is used to fill chronic understaffing, it destabilizes permanent teams, increases the coordination burden, and drives up costs.
Use of temporary hospital staff: a viable complement
The question is not “temporary or no temporary,” but “under what conditions does temporary work remain useful and sustainable?”
What exists today: a cascade approach
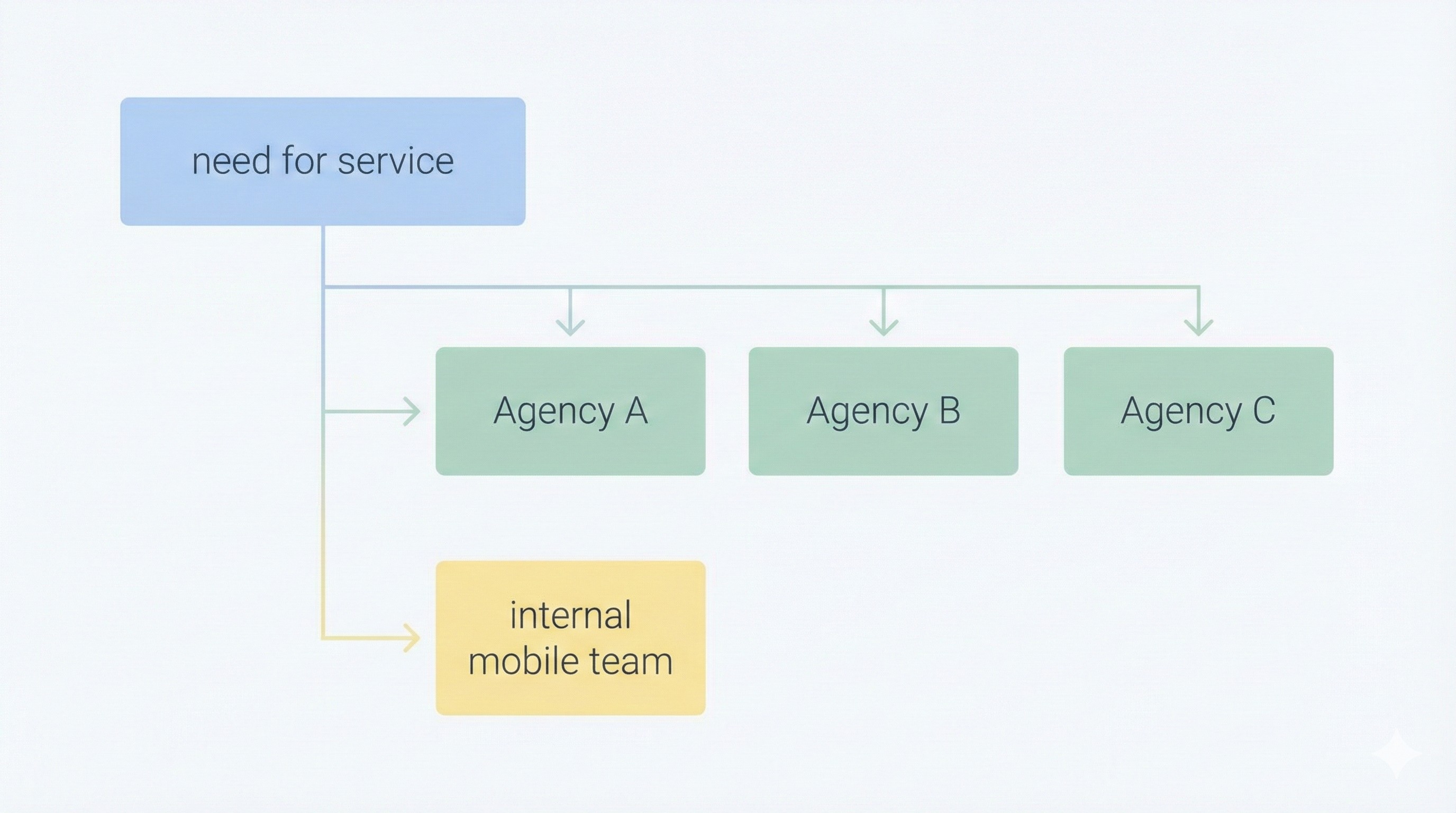
When a department needs extra staff, a healthcare manager submits a request via the dedicated platform. The request follows a cascade approach: it is first sent to the preferred partner agency. If that agency is unable to respond, the request is automatically forwarded to the next agency, and so on.
This system guarantees a high level of responsiveness while maintaining a clear hierarchy of partners. It also provides valuable traceability, which is useful for analyzing the actual volume of external resources used.
At Saint-Pierre University Hospital (Brussels), the internal mobile team is integrated into this mechanism. This makes it possible to quickly mobilize resources already present in the institution before seeking outside help, while maintaining complete visibility on each replacement.
Integrate an internal pool before the external one
Mobilizing the internal network first reduces costs, stabilizes teams, and strengthens belonging.
Better human resources management
The platform provides accurate tracking of external reinforcements. Management teams have an objective view of the number of FTEs mobilized via temporary contracts, service by service. This makes it possible to re-examine structural allocations and gradually move away from management based on “gut feeling.”
For healthcare managers, the benefits are immediate: less administration, greater transparency, and smoother management of unexpected absences. Strategically, it is a lever for correcting areas of dependency and reducing temporary staffing costs by addressing the root causes.
Making dependence on temporary staff visible
Without consolidated data, temporary staffing becomes a habit. With shared indicators, it becomes a controlled choice.
A shared commitment: transparency, recognition, and feedback
From the earliest stages of the project, one key element is established: systematic feedback. Each assignment is followed by mutual feedback: the institution evaluates the agent’s performance, and the professional shares their experience.
This loop promotes:
- Improved interpersonal skills
- Continuous improvement
- A climate of trust between the field, management, and partners
Ultimately, this feedback helps professionalize the replacement relationship, making the use of hospital temporary staff more relevant when it is essential.
Feedback transforms a “stopgap” into an HR lever
Without feedback, we repeat the same mistakes. With feedback, we stabilize and build loyalty.

Conclusion: towards ethical governance of replacement
This project is not just operational. It embodies a freer and more ethical way of thinking about replacement. By centralizing requests and establishing ongoing dialogue, it transforms replacement into a lever for quality of life at work, autonomy, and loyalty.
Caring for those who care also requires tools that serve the collective. It is a matter of restoring meaning to the organization of care, while adopting a clear-eyed approach to shortages and truly shared efficiency.
The use of temporary workers then becomes not a inevitability, but a starting point for building viable and sustainable complementarity.



